Hospitals are no strangers to emergencies. From natural disasters to active shooter events, healthcare facilities face risks that can disrupt operations, endanger lives, and strain resources. In 2025, emergency preparedness has become more critical than ever—driven by lessons from recent real-world hospital incidents.
As facilities managers, security directors, and hospital administrators look ahead, one question remains: What are we learning from these crises, and how can we apply those lessons to improve hospital safety moving forward?
k
k
Why Hospital Emergency Preparedness Looks Different Today
Not long ago, emergency preparedness in healthcare focused mainly on fire drills and weather-related plans. While those remain important, today’s hospitals face a wider and more complex range of threats, including:
-
Workplace violence and active shooters in emergency departments and waiting areas
-
Cybersecurity attacks that can shut down electronic health records and disrupt patient care
-
Severe weather events—including hurricanes, floods, and extreme heat—that test power and backup systems
-
Public health crises, from pandemics to mass casualty events
Each of these emergencies requires coordinated planning between hospital security systems, access control, HIPAA-compliant surveillance, and visitor management.
k
k
Lessons Learned from Recent Hospital Incidents
1. Communication Must Be Instant and Clear
During a hospital shooting incident in 2024, delayed internal communication left staff unsure whether to shelter in place or evacuate. The takeaway? Hospitals need mass notification systems that can send alerts instantly across mobile devices, PA systems, and digital signage.
2. Access Control Saves Precious Seconds
When a tornado struck a Midwestern hospital, zone-based access control kept critical areas—like neonatal intensive care units (NICUs) and pharmacies—locked down, preventing chaos and protecting patients. Controlled access isn’t just about security—it’s also about directing people safely during emergencies.
3. Visitor Management is More Than Check-In
In a 2023 infant abduction case, investigators found that the hospital’s visitor management system failed to flag repeated suspicious entries by the same individual. Modern visitor management in hospitals must track, monitor, and even analyze visitor patterns in real time.
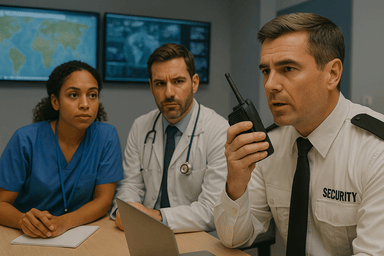
4. Technology and Human Training Go Hand-in-Hand
Even the most advanced hospital security systems can’t replace human decision-making. Hospitals that fared best during recent crises paired strong technology with ongoing security training and drills for staff.
k
k
How Hospitals Can Strengthen Preparedness in 2025
-
Integrate Security Systems – Link access control, surveillance, alarms, and mass notifications into a single command center.
-
Adopt AI-Powered Surveillance – Use intelligent video analytics to detect unusual behavior or crowding before incidents escalate.
-
Regularly Audit Security Protocols – Emergency plans should be living documents, updated after every drill or incident.
-
Plan for Both Physical and Cyber Threats – Hospitals must treat cybersecurity as an essential part of emergency preparedness.
-
Prioritize Staff Safety – Equip healthcare workers with panic buttons, duress alarms, and secure communication channels.
k
k
Conclusion
Emergency preparedness in 2025 isn’t just about having a plan—it’s about building a resilient, secure, and adaptable hospital environment. The lessons from recent incidents are clear: hospitals must combine modern security technology, access control, HIPAA-compliant surveillance, and visitor management policies with well-trained staff to respond quickly and effectively.
At SSP, we understand the unique challenges hospitals face. Our role is to help you integrate systems, strengthen policies, and prepare for the unexpected—so your patients and staff are always protected.
Talk to SSP about securing your healthcare facility and improving your hospital’s emergency preparedness strategy.


